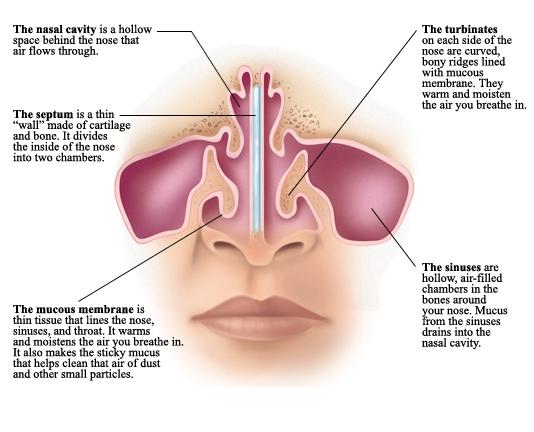
Rhinitis, commonly known as a “stuffy nose”, is the medical term for inflammation of the nasal cavities. The 3 most common causes are infectious (virus and bacteria), non-allergic (vasomotor), and allergic rhinitis.
Allergic rhinitis is very common, affecting roughly 20-25% of the population. The prevalence of allergic rhinitis seems to be increasing as well. It affects both pediatric and adult patients, with most patients presenting with symptoms before 20 years of age.
There are two types of allergic rhinitis, seasonal and perennial. Seasonal occurs primarily during season changes, as the most common allergens are pollens (trees, grasses, and weeds). Perennial allergens, such as dust mites and molds, can cause symptoms all year.
Patients can have symptoms confined to the nasal airway, such as clear rhinorrhea (runny nose), sneezing, and congestion. However, other patients may have other organ involvement, including watery and itchy eyes, skin rash (dermatitis), ear pressure and fluid, and asthma. Many patients also complain of recurrent sinus infections, which may be exacerbated by chronic allergic rhinitis.
The diagnosis of allergic rhinitis can often be made upon patient history and physical examination. However, sometimes formal allergy testing is warranted. There are 2 main types of testing: blood testing and skin testing. Unless contraindicated, skin testing is preferred by most physicians as it is more accurate.
Treatments for allergic rhinitis are aimed to reduce the symptoms of the patient. The best therapy is avoidance of the specific allergen. Eliminating exposure to allergens is the most effective preventive measure, but requires consistent effort. Patients with pollen allergies reduce their exposure by remaining indoors during hay fever season, particularly in the morning and evening, when outdoor pollen levels are at their highest. Patients with dust mite allergy often can “dust-proof” their home by using special air filters, placing special covers on their mattress and pillows, and removing dust-filled reservoirs (carpets, etc)
When patients are unable to eliminate the specific allergens, then medical therapy is warranted. The mainstay of medical therapy is topical medicated nasal steroid sprays and oral antihistamines. Although both have some potential side-effects, each has been proven to be very effective in symptom reduction. However, select patient may need further treatments with formal allergy shots, known as immunotherapy.
A large amount of clinical research has established the effectiveness of immunotherapy in reducing symptoms of patients with allergic rhinitis. Success rates have been demonstrated to be as high as 80-90% for certain allergens. However, it is a long-term process. Typically, noticeable improvement is not observed for 6-12 months, and, if helpful, therapy should be continued for 3-5 years.
Allergic rhinitis is a common medical condition that can cause chronic nasal and sinus problems. However, there are many good treatment options available. Any questions or concerns may be discussed further with your local ENT physician.
Robert Wilson, MD.