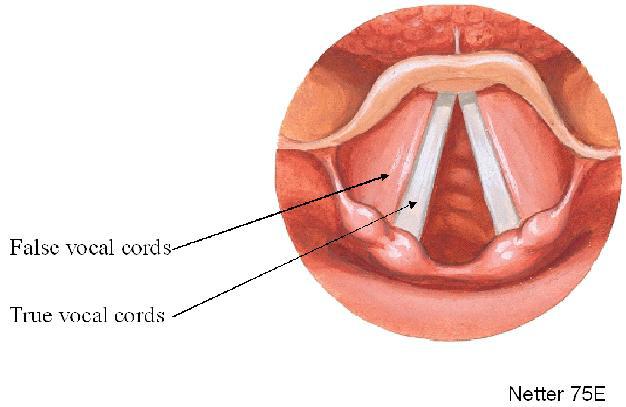
Hoarseness is a general term defined as a change of voice quality. There are many more descriptive terms, such as scratchy, raspy, weak or breathy, or strained. These more specific descriptions can help a physician better determine the cause of the vocal change.
When otolaryngologists discuss hoarseness, one of the most important aspects is the timing of the vocal change. If it has occurred less than 2 weeks, then we define it acute hoarseness; whereas if it has been over 2 weeks, it is defined as chronic hoarseness. Regarding the timing, it is important to note if the voice is worse in the mornings or in the evenings.
Another important piece of the history is whether a patient has used tobacco, which significantly increases the patient’s risk of laryngeal (throat) cancer. A patient who uses tobacco and has chronic hoarseness needs evaluated by an otolaryngologist immediately.
Acute hoarseness is often secondary to laryngitis, or inflammation of the vocal folds. The most common reasons for acute laryngitis are a viral upper respiratory infection and vocal trauma (screaming). The symptoms include a weak and scratchy voice quality associated with a mild sore throat. A viral laryngitis often is accompanied with a cough and a low-grade fever. The treatment for both include conservative treatments, such as Tylenol or Ibuprofen as needed for pain and increased hydration. Patients will need to rest their voice by using “arms-length” speaking, which implies that you should not be too close (whisper) or too far (scream) when talking, for one week.
Chronic hoarseness has many causes, but the most common are related to gastric reflux disease and posterior nasal drainage. These patients often describe their voice as raspy or scratchy. The symptoms are often worse in the mornings due to lying flat in bed, which allows gastric reflux or nasal drainage to irritate the vocal cords all night. Other symptoms besides vocal changes include repeated throat-clearing, a nonproductive cough, and a foreign body (globus) sensation. Most patients do well once the reflux or nasal drainage is treated appropriately.
Patients who use tobacco will often develop chronic laryngitis, secondary to the inflammatory changes produced by the tobacco. They have an increased risk of benign vocal cord lesions, such as polyps. However, more concerning, is the increased risk of cancer development. If a mass or suspicious lesion is identified on exam, then the patient will likely need to go to the operating room for a biopsy using general anesthesia.
Hoarseness that is described as weak or breathy is often due to weakness in vocal fold mobility. Often patients also note trouble swallowing with intermittent spells of choking, mainly with liquids. The most common reasons an adult may have vocal fold weakness are recent intubation (with surgery) or a recent viral infection. However, this could be a sign of something more concerning, such as a chest or lung tumor. Once the underlying problem is identified, the patient can be treated appropriately.
Pediatric patients also may have vocal changes that warrant further evaluation. The most common cause of hoarseness in children is benign vocal nodules, known as “screamer’s nodules”. As the name implies, this is secondary to repeated vocal trauma (screaming). This often resolves over time without any long-term problems. However, there are other causes, such as vocal fold weakness or benign tumors (polyps), which may cause progressive hoarseness or shortness of breath or noisy breathing (stridor). If these symptoms accompany the hoarseness, then the patient may need examined in the operating room for a complete evaluation.
Hoarseness is a very common medical complaint that has many causes. An otolaryngology evaluation maybe needed to fully diagnose and treat the condition, using both medical and surgical treatments.
Robert Wilson, MD.